Last updated: February 16, 2024
16 mins read
- Key Takeaways
- Why Measure Your Inflammation (hs-CRP), and What Does It Mean
- Chronically elevated CRP: A Direct Link to Decreased Longevity
- How can I better understand my results?
- hsCRP vs. CRP
- What are the causes of persistently high baseline CRP?
- Evidence-Based Approaches to Lowering Baseline CRP
- Evidence for commonly suggested dietary and lifestyle changes that lower CRP:
- Evidence for Commonly Used Supplements for Reducing CRP Levels:
- Tracking your hsCRP with SiPhox Health:
Key Takeaways
- Chronic inflammation, detectable through high-sensitivity CRP (hs-CRP) blood tests, is a major contributor to several leading causes of death, including heart disease, cancer, and diabetes. It can be silently harmful for years.
- Chronically elevated CRP levels are linked to an increased risk for noncommunicable diseases and are now recognized as an active cause of inflammation, not just a marker.
- Lifestyle changes, such as improved diet, regular exercise, and quitting smoking, along with certain supplements like curcumin and Omega-3, can effectively lower CRP levels and reduce inflammation.
Why Measure Your Inflammation (hs-CRP), and What Does It Mean
There are two main types of inflammation. Acute (short-term) and chronic inflammation (long-term, low-level).
Classically, inflammation is viewed as an acute response to tissue injury, infection, or another disease state that produces characteristic symptoms (swelling, redness, and warmth). In most cases, this is a functional and useful immune response. However, in some cases, the inflammatory system can be operating at a persistently elevated level, which is known as chronic inflammation.
The medical community has been aware of chronic inflammation for a long time, but only in recent decades has it become possible to track low levels of inflammation using high-sensitivity blood tests. This has shed light on chronic, systemic inflammation as a highly destructive process that drives disease pathogenesis [1] and the aging process itself. It contributes so significantly to the deterioration associated with aging that it has been coined “Inflammaging.” [2]
Chronic inflammation contributes to the development of at least 7 of the 10 leading causes of death in the United States. It may go undetected for years or even decades without proactive tracking, silently threatening your health.
C-Reactive Protein, or CRP, is used to measure acute inflammation, but with the advent of hsCRP (high-sensitivity CRP) testing, it became possible to use it for tracking chronic inflammation as well. CRP is one of several proteins rapidly produced by the liver during an inflammatory response. Its primary goal in acute inflammation is to coat damaged cells and bacteria to make them easier to recognize by other immune cells.
Chronically elevated CRP may signal an increased risk for practically all noncommunicable diseases (NCDs), [3] including heart disease, cancer, diabetes, stroke, Alzheimer’s disease, chronic kidney disease, osteoporosis, chronic lower respiratory disease, and more – even if you are asymptomatic. However, conventionally, it is not treated on its own until it occurs in association with another medical condition (e.g., rheumatoid arthritis.)
CRP, in recent years, has also become understood as an active cause of inflammation in addition to simply being a marker of inflammation.
Chronically elevated CRP: A Direct Link to Decreased Longevity
CRP is an immune system protein produced by the liver in response to injury, infection, or other inflammatory events. Physicians often look at CRP as one of the major markers of chronic and acute inflammation.
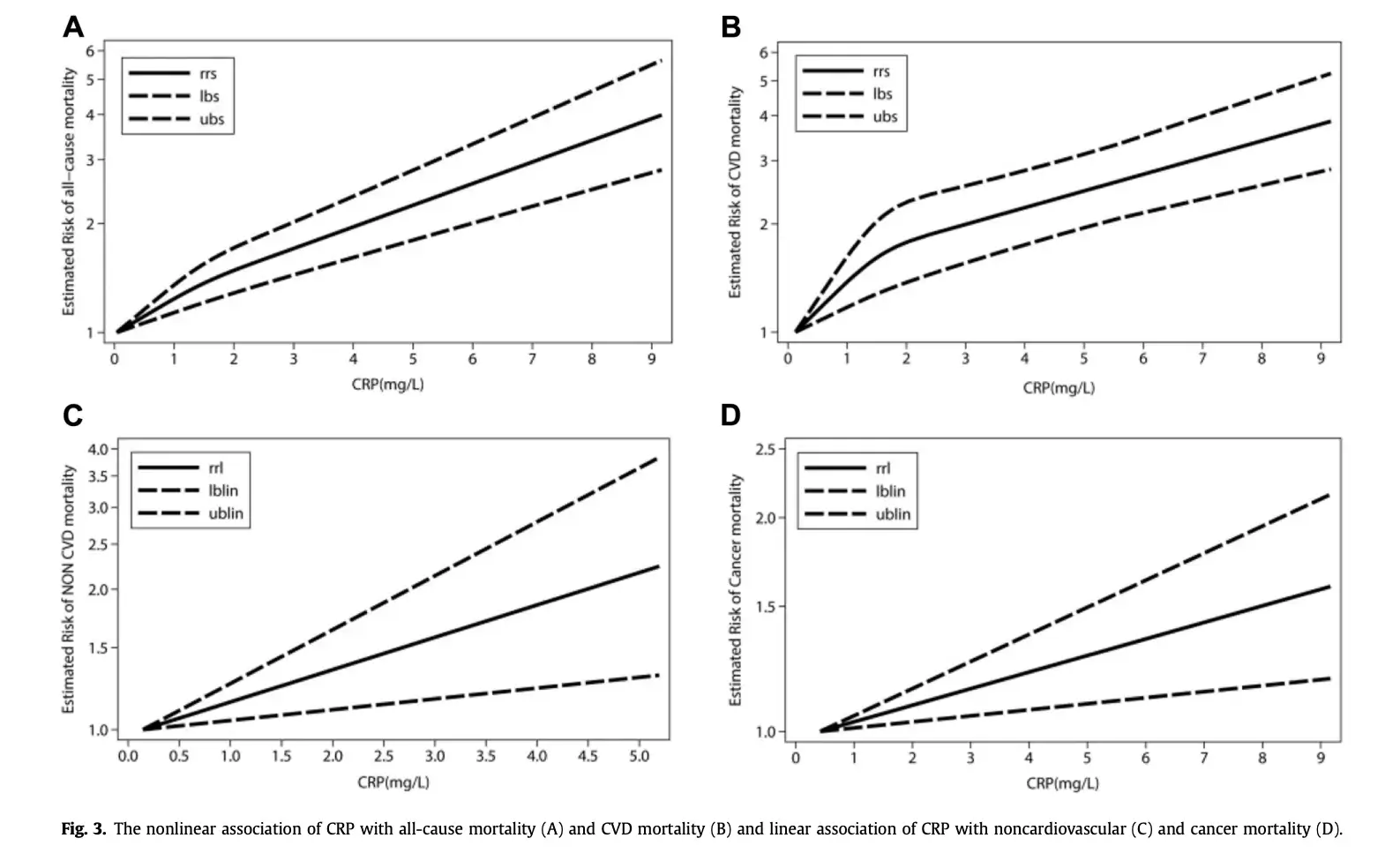
Meta-analyses of all-cause mortality studies find that for longevity, the ideal baseline CRP is essentially as low as possible. [4]
This empirical evidence agrees well with aging clocks like the Morgan Levine PhenoAge clock, [5] where baseline CRP is a major component, and with leading Inflammaging [6] research.
Chronic inflammation is a contributing factor [7] to cancer, heart disease, lung disease, chronic obstructive pulmonary disease, chronic kidney disease, Alzheimer’s disease, and irritable bowel syndrome. It is also connected to an array of metabolic disorders, including pre-diabetes and diabetes, obesity (animal studies suggest that high levels of CRP may even directly cause weight gain [8]by interfering with metabolism), and high blood pressure (CRP causes chronic contraction of blood vessels). [9]
This is why tracking and optimizing baseline CRP using high-sensitivity CRP (hsCRP) tests is just as important for longevity and healthspan as blood glucose tracking (diabetes prevention), and lipid (ApoA1, ApoB, HDL, LDL) tracking (cardiovascular risk reduction).
How can I better understand my results?
The CDC/AHA divides the risk of cardiovascular events into the 3 following categories[10]
- Low risk: less than 1.0 mg/L
- Average risk: 1.0 to 3.0 mg/L
- High risk or acute inflammation: above 3.0 mg/L (consider discussing with your physician
It is important to note that research supports targeting baseline CRP levels below 0.5 mg/dL. Commonly, lab tests will report “<0.2 mg/L” if you have an ideal/ undetectable value.
For example, a study [11] of 27,939 women, showed that hsCRP and cardiovascular risk are proportional, meaning that lower hsCRP was linked to reduced risk—even at the lowest levels measured (<0.5 mg/L).
hsCRP vs. CRP
You may have seen CRP and hsCRP in your test results. These both refer to the same inflammation protein. CRP, or C-reactive protein, is also called “standard CRP.” CRP is also used in the diagnosis of severe inflammation related to acute conditions. The standard CPR test measures it in the range of 10 to 1000 mg/L. An hsCRP or “high sensitivity CRP” accurately detects lower levels of the protein and is used to evaluate individuals for low-grade inflammation and risk of heart disease. hsCRP measures CRP in the range from 0.2 to 10 mg/L.
Note: A high CRP value alone cannot be used to diagnose any specific issue. Consult your physician for any interpretation of your CRP test results.
What are the causes of persistently high baseline CRP?
Short-term CRP can spike for many reasons including intense exercise, infection, and other factors. Putting those aside, persistently elevated CRP (e.g. above 1mg/L) can have many underlying causes.
Nearly every common chronic disease has an inflammatory component. Even mental health conditions such as anxiety and depression tend to be associated with elevated CRP. [12] As scientists learn more about the brain-body relationship, new connections of this type between blood biomarkers and mental health conditions are being found.
Chronic inflammation can last for months or indefinitely. It can be driven by underlying issues including pathogens (like a fungus or parasite), foreign material (such as a toxic chemical), or autoimmune disorders (like IBD or rheumatoid arthritis). However, for many modern Americans, lifestyle factors [13] such as poor diet, nutritional or hormonal imbalance, cigarette, and alcohol use, and disrupted sleep can be the main driver of long-term inflammation.
Evidence-Based Approaches to Lowering Baseline CRP
Proactively making an effort to lower CRP levels is both feasible and recommended. Lifestyle has a direct impact on CRP levels. For example, the consumption of trans-fatty acids can increase CRP levels [14] within the 0.9 – 2.3 mg/L range. Whereas moderate exercise has been shown to be a means of lowering high CRP. [15]
Below are diet, lifestyle, and supplementation protocols that have strong evidence (references included) for improving elevated baseline CRP levels. Note that where possible we generally only reference Randomly Controlled Studies (RCTs) and Meta-analyses of RCTs.
Note: The information below is provided for reference, please consult your physician before starting any new health regimen.
Evidence for commonly suggested dietary and lifestyle changes that lower CRP:
- Improved sleep
- Complete and partial sleep deprivation has been shown to increase CRP levels in healthy adults.[16]
- SiPhox user data shows a strong -0.46 inverse correlation between the SiPhox sleep score (based on wearable device sleep data) and hsCRP.
- Top SiPhox sleep insight:
“Consider leaving your smartphone and any other screens outside your bedroom before going to bed. This will help you fall asleep faster and improve your sleep efficiency.”
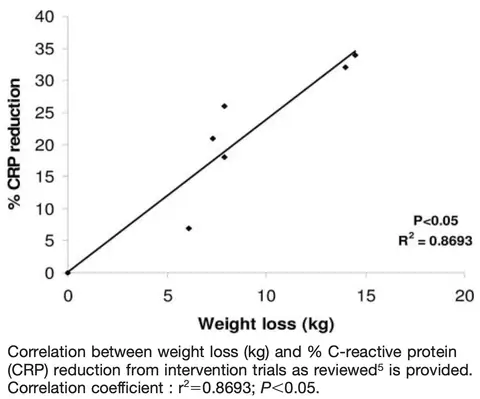
- Weight loss (if overweight) and improved diet
- Following a Mediterranean-style diet for a duration of 12 weeks has been shown to decrease CRP levels.[17]
- Weight loss is correlated with lowered CRP levels.
- Exercise
- Medium-intensity exercise (20 minutes to 1 hour of running) is known to lower your CRP levels[18]
- SiPhox user data shows a significant -0.3 inverse correlation between daily steps taken (based on wearable device activity data) and hsCRP.
- Cessation of smoking
- When levels of CRP were compared in smoking status groups for 1926 men aged 40 to 69 years, it was found that long-term cessation brought CRP levels down to non-smoker levels.[19]
- Removal of processed foods and refined sugars from your diet
- A low-glycemic index and low glycemic load diet (eating less simple carbohydrates and lower portions of carbs) has been shown to decrease CRP levels.[20]
- Heat Exposure
- Sauna usage [4-7x a week for 10-15 minutes] is associated with decreased hs-CRP levels.[21]
Evidence for Commonly Used Supplements for Reducing CRP Levels:
- Curcumin
- (0-3 mg per kilogram of body weight, or roughly 0-1.4 mg per pound.) supplementation is associated with lower CRP levels.[22][23]
- Zinc
- A meta-analysis of 35 Randomized Control studies comprising 1995 participants has displayed a decrease in CRP following Zinc supplementation. [24]
- Vitamin D
- Increasing sun exposure (15-20 minutes a day) or supplementing with Vitamin D over the counter may increase your Vitamin D levels and increase your Inflammation Score.[25]
- Omega 3
- Omega 3 or fatty fish consumption is associated with lower CRP levels.[26]
- Probiotic
- Probiotic supplementation has been shown to decrease CRP levels in a meta-analysis of 31 studies.[27]
- Vitamin E (alpha-tocopherol)
- Supplementing vitamin E (15mg/day) can lower inflammation. A meta-analysis of 246 participants suggests that supplementation with vitamin E in the form of either α-tocopherol or γ-tocopherol would reduce serum CRP levels.[28]
- Quercetin
- Supplementing quercetin at doses above 500 mg/day can lower inflammation levels. This meta-analysis showed a significant effect of quercetin supplementation on the C-reactive protein-especially at doses above 500 mg/day and in patients with CRP <3 mg/l.[29]
Note: All of the lifestyle, diet and supplementation approaches to lowering chronic inflammation have been shown to work for the average person. To know which ones work for you, tracking your hsCRP on a regular basis is the most effective approach.
Tracking your hsCRP with SiPhox Health:
- At-home kit delivered to your home
- Fingerprick sample self-collection (low-pain, adjustable lancets)
- $295 one-time or subscribe to get $85 per test*
- Number of biomarkers included: 17 (4 inflammation markers including hsCRP)
- Sleep and activity tracking: Included, 200 devices supported
- 2-5 business days after collection
Revolutionizing hsCRP tracking:
SiPhox Health is developing next-generation at-home testing hardware that will deliver biomarker results, including hsCRP, in under 10 minutes using only 5 microliters of blood, similar to a glucometer. This advancement will reduce the cost, time, and difficulty of tracking hsCRP by a factor of ten. Read more here.

*Subscription fee of $24/month, plus $85 per test
Disclaimer: If you have any medical questions or concerns, please talk to your healthcare provider. The articles on the SiPhox Health Hub are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis or treatment.
References





